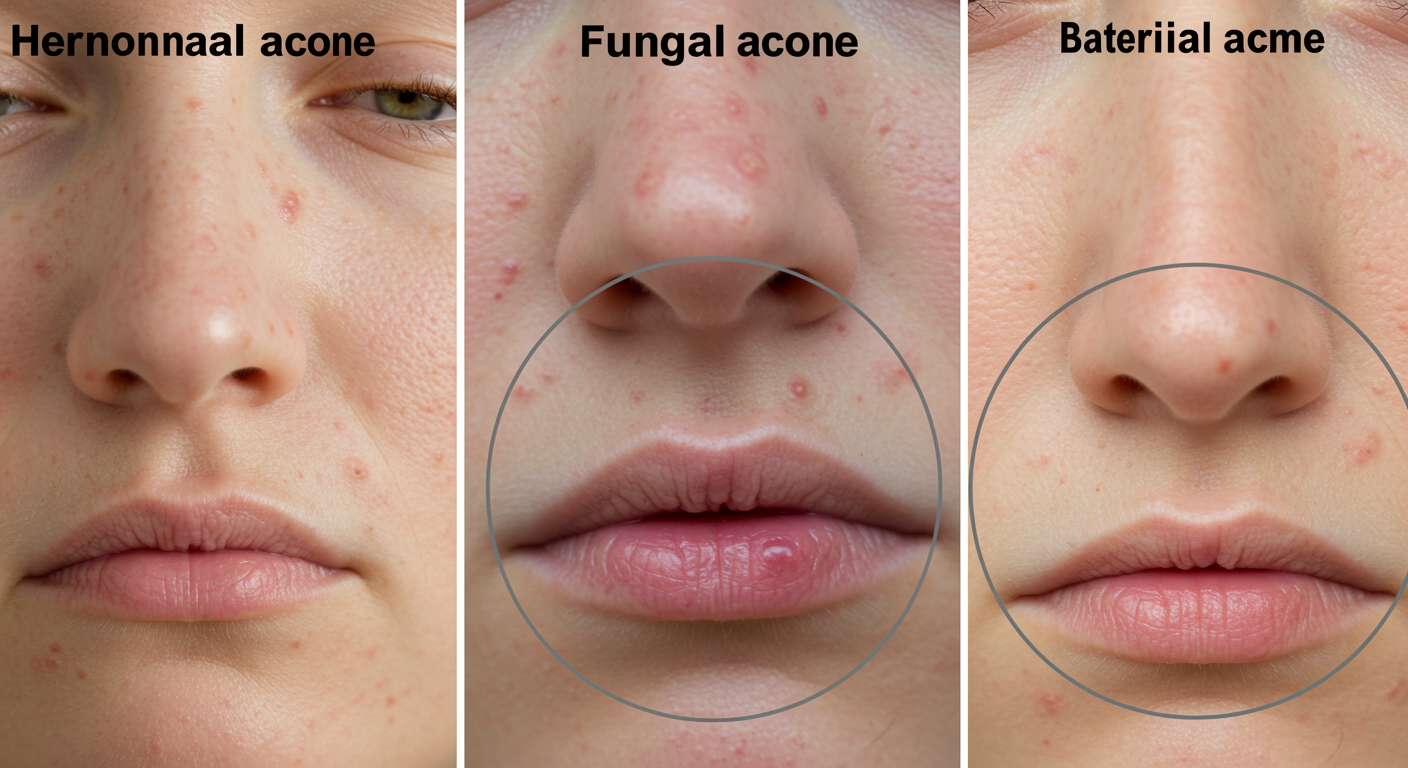
Hormonal vs Fungal vs Bacterial Acne
Hormonal vs Fungal vs Bacterial Acne: How to Tell the Difference
Not all acne is the same—and treating the wrong type can make breakouts worse. If you’ve tried every cleanser, serum, or spot treatment with little success, your acne may not be “stubborn” at all—it may simply be misidentified.
This guide breaks down the key differences between hormonal acne, fungal acne, and bacterial acne, including how they look, where they appear, what triggers them, and how to support your skin naturally—without damaging the skin barrier.
This article is part of our Skin School → Acne Solutions series. If your skin is also reactive or easily irritated, review our Sensitive Skin Care Routines before introducing new products.
Why Identifying Your Acne Type Matters
Acne treatments are not one-size-fits-all. Products designed for bacterial acne can worsen fungal acne, while harsh actives used for oil control can disrupt hormonal or sensitive skin.
Correctly identifying your acne type helps you:
- Avoid unnecessary irritation and barrier damage
- Choose ingredients your skin actually responds to
- See results faster with fewer products
What Is Hormonal Acne?
Hormonal acne is driven by internal hormone fluctuations—most commonly androgens—which increase oil production and inflammation.
Common Signs of Hormonal Acne
- Deep, tender, or cystic breakouts
- Flares around the jawline, chin, and lower cheeks
- Worsens before menstruation or during stress
- Breakouts feel sore rather than itchy
Hormonal acne often persists into adulthood and may not respond to typical “acne-fighting” products alone.
What Is Bacterial Acne?
Bacterial acne is caused by the overgrowth of Cutibacterium acnes, a bacteria that thrives in clogged pores and excess oil.
Common Signs of Bacterial Acne
- Inflamed pimples, pustules, or cysts
- Varied sizes and shapes
- Redness and tenderness
- Often improves with antibacterial ingredients
Over-cleansing or stripping the skin can actually worsen bacterial acne by disrupting the skin’s microbiome.
What Is Fungal Acne?
Fungal acne—more accurately called Malassezia folliculitis—is not true acne. It’s caused by an overgrowth of yeast that feeds on oils and occlusive ingredients.
Common Signs of Fungal Acne
- Clusters of small, uniform bumps
- Often itchy or irritated
- Appears on the forehead, chest, back, or shoulders
- Worsens with sweat, heat, or heavy oils
Fungal acne does not respond to traditional acne treatments and can worsen with certain moisturizers or antibiotics.
Hormonal vs Fungal vs Bacterial Acne: Quick Comparison
| Feature | Hormonal | Bacterial | Fungal |
|---|---|---|---|
| Main Cause | Hormone fluctuations | Bacterial overgrowth | Yeast overgrowth |
| Appearance | Deep, cystic | Inflamed pimples | Small, uniform bumps |
| Itchiness | No | No | Yes |
| Location | Jawline, chin | Face, back | Forehead, chest |
Can One Person Have Multiple Acne Types?
Yes. Many people experience mixed acne—for example, hormonal acne on the jawline and fungal acne on the forehead. This is why gentle, barrier-supportive routines matter.
If your skin also shows signs of irritation, redness, or dryness, your acne may overlap with a damaged barrier. Learn more in our guide: Sensitive Skin vs Damaged Barrier vs Eczema .
How to Treat Acne Without Damaging Your Skin Barrier
No matter the acne type, over-exfoliation and harsh treatments can worsen breakouts long-term.
- Use gentle, non-stripping cleansers
- Avoid stacking too many actives
- Support the barrier with hydrating ingredients
- Patch test new products first
If breakouts persist alongside dryness or sensitivity, prioritize barrier repair: Skin Barrier Repair Routine (AM + PM).
People Also Ask
How do I know if my acne is hormonal, bacterial, or fungal?
Hormonal acne is deep and cyclical, bacterial acne is inflamed and varied, and fungal acne appears as itchy, uniform bumps—often worsening with sweat or humidity.
Can doxycycline cause fungal acne?
Yes. Antibiotics can disrupt the skin microbiome, allowing yeast to overgrow and trigger fungal acne—especially on the chest or back.
How do you tell if acne is bacterial or fungal?
Bacterial acne varies in size and responds to antibacterial care. Fungal acne is uniform, itchy, and worsens with oils or occlusives.
Can hormonal acne look like fungal acne?
Yes, but itchiness and treatment response help differentiate them. Hormonal acne is tender; fungal acne often itches.
Explore the Complete Acne-Prone Skin Routine
Clearer-looking skin requires more than a single product — it requires a balanced, toxin-free skincare routine for acne-prone skin. At Glimmer Goddess®, we design our formulations using Certified Organic Ingredients to support barrier repair, reduce inflammation triggers, and maintain hydration balance.
To build your full routine, explore:
- Toxin-Free Skincare Routine for Acne-Prone Skin
- Best Ingredients for Acne-Prone Skin
- What Acne-Prone Skin Should Avoid
- Non-Comedogenic Oils Explained
Every Glimmer Goddess® formula is handcrafted in Texas and created to support long-term skin clarity without harsh chemicals.
References
- American Academy of Dermatology — Acne types and treatment guidance
- Cleveland Clinic — Hormonal acne and adult acne insights
- DermNet — Malassezia folliculitis clinical overview
- PubMed — Acne pathophysiology and microbiome research
Handcrafted in Texas.



